Background/Methods: The two-step approach to HI HSCT was developed in 2005 with the first patient treated on clinical trial in early 2006. In this approach, after myeloablative [MA- 12 Gy total body irradiation (TBI)], reduced intensity (RIC- fludarabine, 2 Gy TBI and cytarabine, OR thiotepa, OR busulfan), or nonmyeloablative (NMA-fludarabine and 2 Gy TBI) conditioning, patients receive a fixed dose of unmanipulated donor lymphocytes (DLI) containing 2 x 108/kg CD3+ cells (Step 1). Two days later, cyclophosphamide (CY) 60 mg/kg/day x 2 is infused for bidirectional T cell tolerization. One day after the completion of CY, a CD34-selected stem cell product is infused (Step 2). All patients receive tacrolimus and mycophenolate mofetil starting at d-1. The two-step approach avoids stem cell exposure to CY, allows a growth factor-naïve fixed dose of donor T-cells to be infused increasing uniformity for outcomes analysis, and permits easier manipulation of both T-cell and CD34 cell dosing. In later protocols, the timing of the DLI after conditioning and the CD34 cell dose have been manipulated with the goal of reducing relapse, and age-based comorbidity and performance status indices were added to eligibility criteria to reduce non-relapse mortality (NRM).
Results: We analyzed all 283 patients treated on a two-step HI HSCT clinical trial at our institution. The median follow-up is 63 (range 1-165) months. Diagnoses were AML (n=118), MDS (n=43), myeloproliferative disorder (n=7), CMML (n=3), B-ALL (n=21), Ph+ ALL (n=15), multiple myeloma (n=14), T cell ALL (n=9), aggressive lymphoma (n=15), CLL (n=8), Hodgkin (n=7), aplastic anemia (n=5), and lymphoma-other (n=18). Patients had high (45%), intermediate (43%), very high (5%), and low (4%) risk disease per the Revised Disease Risk Index. Median age of the group is 58 (19-78) years and 21% of patients were >age 65. Conditioning was MA in 56%, RIC in 37%, and NMA in 7%. All patients received 2 x 108/kg CD3+ cells in step 1 of the HSCT except for 1 early patient who received 1.7 x 108/kg CD3+ cells. Median CD34 cell dose was 6.3 (range 1.0-20.0) x 106/kg, median non-CY-exposed T cells in the CD34 product was 2.88 (range 0.33-50.0) x 103/kg.
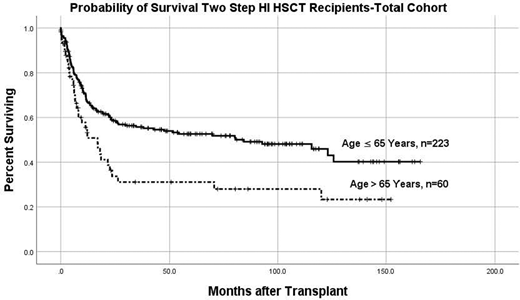
Patients developed a haploimmunostorm manifested by high grade fever, diarrhea and rash within 24 hours of receiving DLI. These symptoms effectively resolved after the administration of CY. Median peak fever of patients during the haploimmunostorm was 103.6 (range 98.6-106.1). No patients died as a consequence of the haploimmunostorm. Cumulative incidence (CI) of donor engraftment was 97%. Median time to neutrophil and platelet engraftment was 11 (8-21) days and 17 (10-173) days respectively. All results at 2 years: CI of relapse and NRM were 25% each. CI grades 2-4 and 3-4 acute GVHD were 39% and 7% respectively, and CI chronic GVHD was 15%. Probability of survival (OS) was 55% in the total cohort and 34% in patients >65 years. In patients with AML which represented the largest subgroup of patients, OS was 51% in the total cohort and 40% in patients > 65.
Conclusion: HI HSCT using the two-step approach is an effective treatment for a variety of hematologic malignancies and dyscrasias. Despite older age, over 1/3 of patients >65 years were alive 2 years after HI-HSCT.
Flomenberg:Tevogen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal